An obscure but important player in the health care industry is in the crosshairs of Montana elected officials, who are proposing new regulations aimed at reducing the cost of prescription drugs.
State Insurance Commissioner Matt Rosendale, an elected Republican, asked state lawmakers Friday to consider additional rules on the contracts between health insurance companies and what he refers to as the middlemen of the pharmaceutical drug industry.
"Right now the three largest PBMs control 85 percent of the pharmaceuticals. We're talking big, big money folks," Rosendale says.
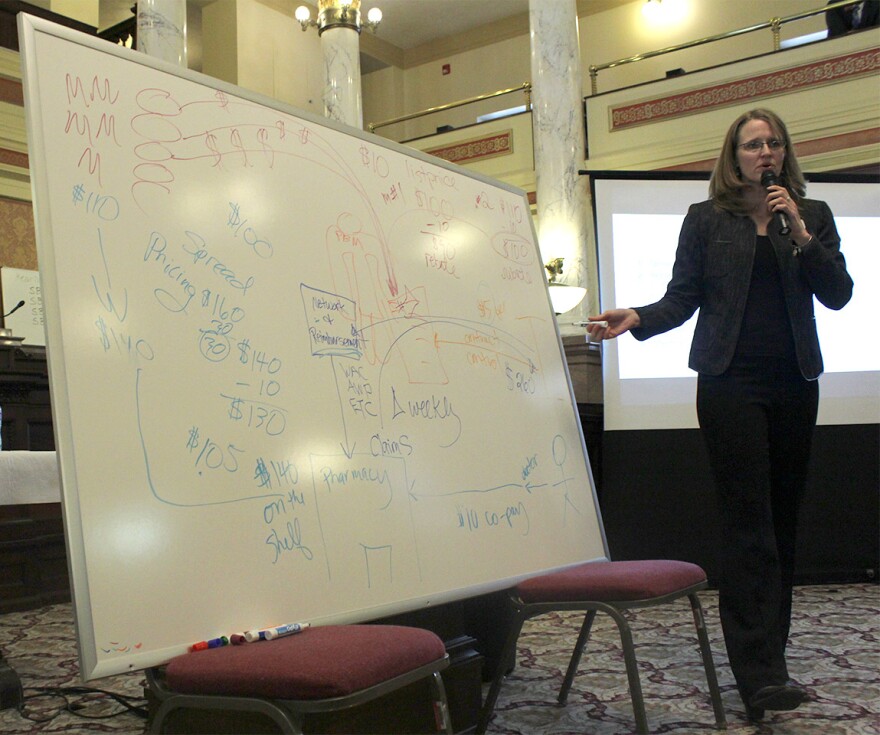
PMBs are pharmacy benefit managers. They negotiate deals between insurance companies, drug manufacturers, retail pharmacies, and government health plans. Those deals along the prescription drug supply chain are often complicated and opaque.
Critics say that leaves room for PBMs to profit from charging unfair prices, but PBM companies say the deals they strike actually lower drug costs.
Janell Williams with the State Auditor’s Office says Senate Bill 71 would regulate contracts between health insurers and PBMs in a way that would prevent PBMs from skiming additional money off their deals.
"It requires that the amount that a health insurer pays for a prescription be the same amount that the pharmacy receives for the drug, no spread," Williams said.
An example of a pharmacy benefit manager using spread pricing would be if the PBM negotiated a deal with a retail pharmacy to sell a medication for $30, but then tells the an insurance company it costs $50.
Shining a light on, or trying to regulate, the pharmaceutical supply chain is difficult. Courts have ruled that federal law preempts some state imposed guidelines for PBMs. But Rosendale’s office says it’s come up with a way around that that could survive a potential legal challenge.
Although Rosendale’s office says the end result of their legislation is to change the behavior of PBMs, nowhere in the bill is "pharmacy benefit manager" or "PBM" written.
The bill directly regulates insurance companies, reaching through them to get PBMs. That has three of Montana’s biggest health insurance companies worried.
"It is of great concern to us that we could be fined for the actions of another party,” says Richard Miltenberger, the chief executive officer of the Montana Health Co-Op.
Miltenberger says his company already doesn’t allow spread pricing and kickbacks that can inflate the cost of prescription drugs.
"We’re going to be paying the PBM, we’re going to tell them they can’t do certain things, we’re going to audit them, but at the end of the day if they do them, we get the fine. And that’s our members’ money.”
Montana Health Co-Op and Pacific Source Health Plans both told lawmakers that drug costs are a big part of the cost of premiums.
Jennifer Hensley with Pacific Source says PBMs help lower drug prices. She says it’s another part of the supply change that deserves the scruity: drug manufacturers.
"Because they’ve done a fantastic job nationwide of turning our lense toward PBMs, away from their own cost-fix cost-gouging practices.”
Pharmacy benefit manager companies also object to the bill. They say it will tie their hands during negotiations and lead to higher drug costs.
But Marc Whitacre, a doctor in Havre, says PBMs use policies like rebates, clawbacks, and spread pricing to make their companies money, and as a result, significantly increase the price his patients pay.
“It’s gotten to the point where what would have been a $4 eye drop to treat a patient after a cataract surgery, is now routinely priced at over $40 when a patient goes to an insurance-carrier approved pharmacy.”
Both Republicans and Democrats on the Senate Business, Labor, and Economic Affairs committee have given indications they will support the bill.
The proposed new regulations would only apply to the market for individual health insurance plans in Montana, which make up less than 10 percent of all policies. Far more Montanans get health coverage through plans from their employers or government plans like Medicare and the VA. The bill, carried by Republican Albert Olszewski was not immediately voted on today.
A separate bill considered by its sponsor as a companion to SB 71, that targets PBMs relationships with retail pharmacies, was unanimously approved by the Senate earlier this week.



